CVS Health® provides the info on the next page. Aetna® is part of the CVS Health family of companies. If you want to stay on our site, choose the “X” in the upper right corner to close this message. Or choose “Go on to next website” to move forward to CVS.com.
Incentives for high-quality care
Incentives for high-quality care
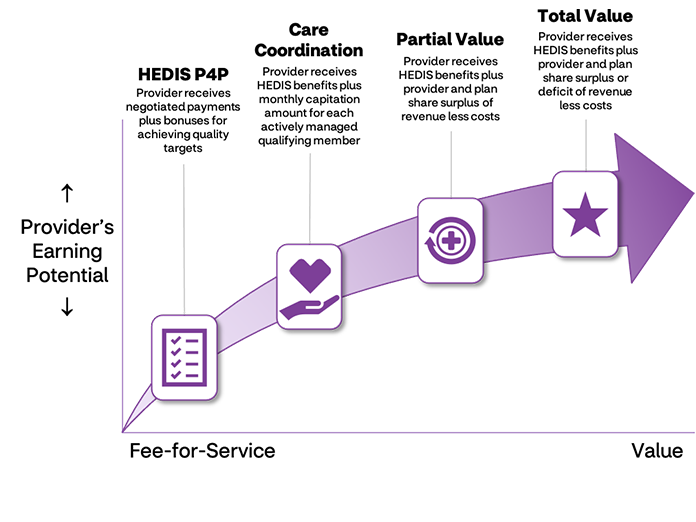
You can earn incentives for providing high-quality, efficient care in all payment models, and you can even share financial risk in some.
VBP has also become a point of focus for the Louisiana Department of Health. The department is moving toward innovative approaches to care coordination, population health management and VBP.
We're used to a health care system that takes care of people after they're already sick. The aim of VBP is to:
- Improve the member's health care experience
- Improve the health of individuals and populations
- Reduce the costs of health care
- Increase provider satisfaction
To meet these goals, VBP moves beyond sick care and adopts a proactive, comprehensive and data-driven approach to keeping people healthy.
HEDIS® Pay for Performance (P4P)
HEDIS is the Healthcare Effectiveness Data and Information Set — standardized performance measures developed by the National Committee for Quality Assurance (NCQA) for the managed care industry. Providers can use HEDIS data to ensure appropriate care for members by identifying and eliminating gaps in care.
We offer all providers the opportunity to take part in our HEDIS P4P program. The program pays providers annual bonuses based on the measures they complete. Each measure has a specific incentive amount paid after a target score is achieved. P4P enhances quality of care by incentivizing providers to focus on preventive and screening services.
Care coordination
To promote diligent and proactive engagement of members, we offer primary care physicians (PCPs) the opportunity to earn incentives by committing to rigorous care coordination in partnership with our care management team.
Providers who take part are eligible to receive a monthly capitation amount for each member (PMPM) assigned to a provider as their PCP with an active provider-patient or provider-client relationship. Providers taking part are required to have regularly scheduled meetings with our care management team to:
- Review selected member cases and progress
- Ensure active management of all members
Provider must meet program expectations to remain eligible for the PMPM fee.
Partial value
To further encourage preventive care, we give providers the option to take part in partial-value shared savings agreements. Providers who achieve a medical benefits ratio* (also known as medical loss ratio) goal we set are paid part of the surplus related to their assigned members’ cost of care. These agreements incentivize providers to actively engage members in preventive, low-cost outreach and care to prevent high-cost emergency department (ED) visits and inpatient admissions.
Providers who take part in a partial-value-based agreement will have more supports and resources, including robust and regular bi-directional data sharing with us. We expect these providers to progress to total-value-based agreements after one to two years.
Better health at lower costs: Why we need value-based care now (PDF)
Total value
The total-value program is the pinnacle of earning opportunities we offer. Providers taking part in total-value-based agreements have the opportunity to earn a greater part of surplus payments than those in partial-value-based agreements, while also being accountable for members' costs.
Each year, providers in total-value-based agreements are paid part of the surplus or pay us part of the deficit related to their assigned members' cost of care.
As with partial-value-based agreements, total-value-based agreements incentivize preventive, low-cost outreach and care to prevent high-cost, high-risk ED visits and inpatient admissions. Providers in total-value-based agreements have access to advanced resources, data sharing and reporting.
Questions?
You can get more info on these payment models. Just email Provider Relations at LAProvider@Aetna.com.
*Medical benefit ratio (MBR) is calculated as the sum of assigned members’ medical expenses divided by the sum of assigned members’ premium revenue.
HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).

