Aetna Better Health does not provide the info on the next page. If you don’t want to leave our site, choose the “X” in the upper right corner to close this message. Or choose “Go on to next website” to move forward.
Value-based care

Value-based care
We’re used to a health care system that takes care of people after they’re already sick. Value-based care (VBC) moves beyond sick care and takes a proactive, comprehensive, data-driven approach to keeping people healthy.
VBC is a health care delivery model that:
- Pays providers based on the health outcomes of their patients and the quality of services they provide
- Focuses on preventive services and chronic disease management to improve members’ quality of life
The goal of VBC is to:
- Enhance the member’s health care experience
- Improve the health of individuals and populations
- Reduce the costs of health care
- Increase provider satisfaction
VBC benefits
VBC benefits
Provider benefits
- Significant financial incentives allow you to reinvest in your practice
- Increased data sharing between payor and provider helps identify risk and improve care coordination
- Pay is based on quality care and improving patient outcomes
- Best practices and infrastructure create foundation for long-term success
Member benefits
- Members are at the center of the health care experience
- Care is proactive, focused on preventive care, managing chronic conditions and keeping member healthy
- Providers are more well-informed and accountable for high-quality outcomes
- Treatment is customized at the member level

Our program at a glance
24 distinct provider groups
40% of membership and 26% of total Medicaid spend by VBC
Nearly 1,200 providers across all regions of the state
- Minimum quality and engagement thresholds for each payment model to ensure needed care is delivered
- 3.0 Value-Based Solution (VBS) Reporting Suite uses actionable data to make sure patients receive the care they need.
- Financial and quality targets based on provider-specific population create a fair baseline for meaningful quality improvement and cost reduction.
- Cross-functional work groups including medical management, quality, pharmacy and network collaborate to establish best practices.
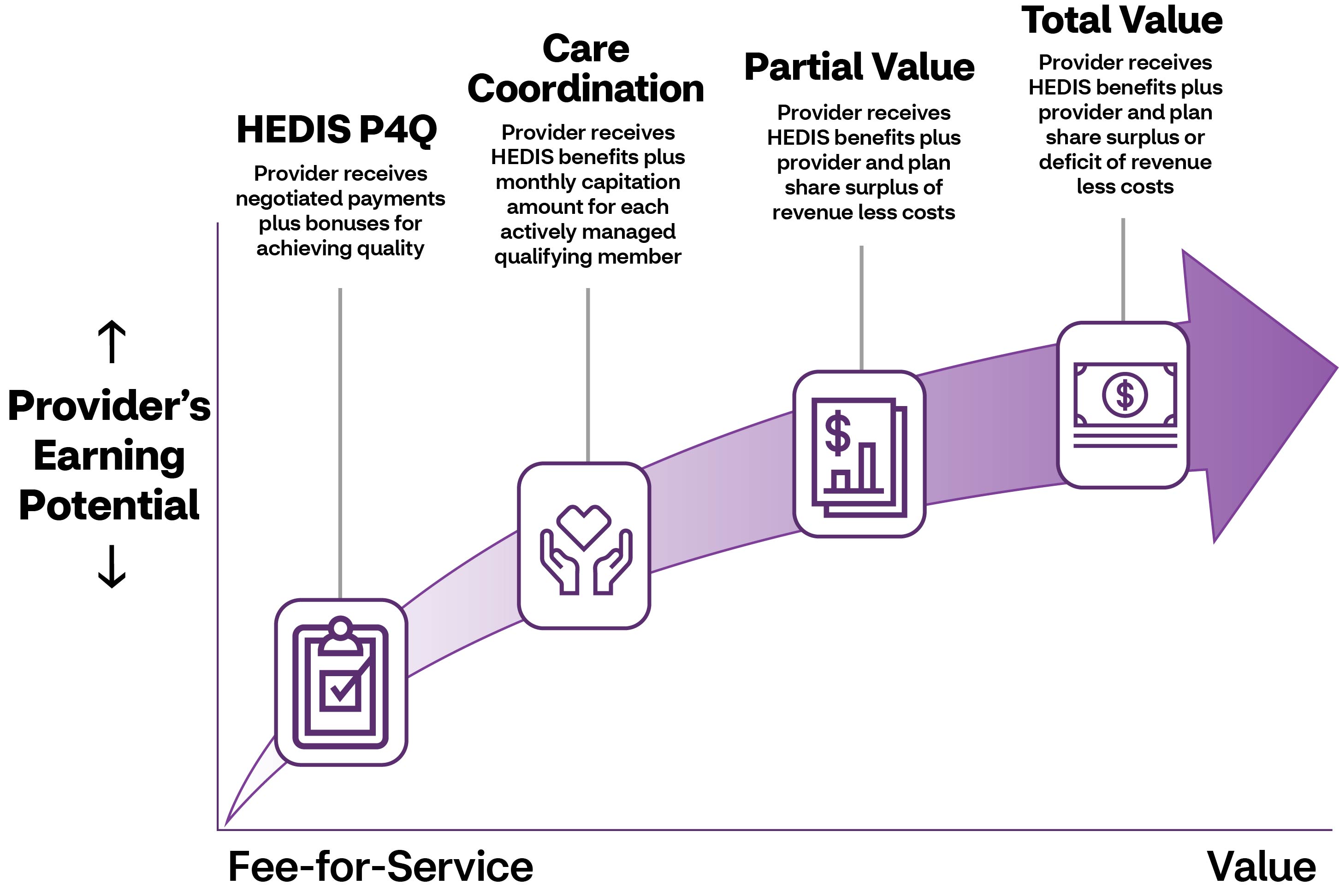
VBC payment continuum
If you’ve ever had the flu, you know how bad it can be. Getting the flu shot is one way to help prevent against the flu, and it's covered by your health plan. The other way is to understand flu myths and facts, so you can stay healthy.
Be prepared for flu season
A flu vaccine (shot) is your best chance to avoid the flu. It’s best to get a shot each year, as soon the flu shot is available in your area. This can be done at your doctor’s office or a health clinic.
The flu vaccine is available in several forms. Most are given in an arm muscle with a needle. Talk with your doctor about which form is best for you.
Myth vs. Fact
M: You can catch the flu from the flu shot
F: A flu shot cannot cause the flu virus.1 The Centers for Disease Control and Prevention (CDC) recommends a yearly flu vaccine for just about everyone ages 6 months and older. If you're not sure if you should get the flu shot, check with your doctor first.
M: The flu shot is expensive.
F: The flu shot is covered by your health plan. If you're enrolled, make sure you get your flu shot at no extra cost.
M: The flu shot shouldn't be given at the same time as other vaccines.
F: The flu shot can be given at the same time as other vaccines,2 including the pneumococcal vaccine.
M: Getting the flu shot is all you need to do to protect yourself from the flu.
F: Getting the flu shot is one way to protect yourself. Make sure you also avoid contact with people who have the flu. And remember to wash your hands often.
M: Antibiotics help with the flu.
F: Antibiotics don't necessarily treat the flu. They only help with infections caused by bacteria. Antiviral drugs like TAMIFLU® can fight the flu virus, so you can feel better faster.
1Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). Misconceptions about seasonal flu and flu vaccines. September 25, 2018. Available at: cdc.gov/flu/prevent/misconceptions.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fflu%2Fabout%2Fqa%2Fmisconceptions.htm. Accessed May 20, 2019.
2Georgia Department of Public Health. Adult influenza and pneumococcal vaccines FAQ.
Available at: dph.georgia.gov/sites/dph.georgia.gov/files/Immunizations/Flu-Season-Flu-Pneu-FAQs.pdf. Accessed May 20, 2019.
HEDIS is the Healthcare Effectiveness Data and Information Set — standardized performance measures developed by the National Committee for Quality Assurance (NCQA) for the managed care industry. Providers can use HEDIS data to ensure appropriate care for members by identifying and eliminating gaps in care.
We offer all providers the opportunity to take part in our HEDIS P4P program. The program pays providers annual bonuses based on the measures they complete. Each measure has a specific incentive amount paid after a target score is achieved. P4Q enhances quality of care by incentivizing providers to focus on preventive and screening services.
To promote diligent and proactive engagement of members, we offer primary care providers (PCPs) the opportunity to earn incentives by committing to rigorous care coordination in partnership with our care management team.
Primary care providers who take part can receive a monthly capitation amount for each assigned member (PMPM) with an active provider-patient relationship. Providers taking part are required to have regularly scheduled meetings with our care management team to:
- Review selected member cases and progress
- Ensure active management of all members
Providers must meet program expectations to remain eligible for the PMPM fee.
To further encourage preventive care, we give providers the option to take part in partial-value shared savings agreements. Providers who achieve a medical benefits ratio* (also known as medical loss ratio) goal we set are paid part of the surplus related to their assigned members’ cost of care. These agreements incentivize providers to actively engage members in preventive, low-cost outreach and care to prevent high-cost emergency department (ED) visits and inpatient admissions.
Providers who take part in a partial-value-based agreement will have more supports and resources, including robust and regular bi-directional data sharing with us. We expect these providers to progress to total-value-based agreements after one to two years.
The total-value program is the pinnacle of earning opportunities we offer. Providers taking part in total-value-based agreements can earn a greater part of surplus payments than those in partial-value-based agreements, while also being accountable for members’ costs.
Each year, providers in total-value-based agreements are paid part of the surplus or pay us part of the deficit related to their assigned members’ cost of care.
As with partial-value-based agreements, total-value-based agreements incentivize preventive, low-cost outreach and care to prevent high-cost, high-risk ED visits and inpatient admissions. Providers in total-value-based agreements have access to advanced resources, data sharing and reporting.
Questions?
You can get more information on these payment models and request the 2024 Value Based Program Booklet. Just email Provider Relations.
*Medical benefit ratio (MBR) is calculated as the sum of assigned members’ medical expenses divided by the sum of assigned members’ premium revenue.
HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).
